Cystitis- This is a pathology, characterized by the development of an inflammatory process that affects the wall of the bladder as a result of the effects of bacterial microorganisms.
Statistical cystitis- One of the most common urological pathologies. Women are predisposed much more to the occurrence of this inflammation, due to their Morphophysiological features.
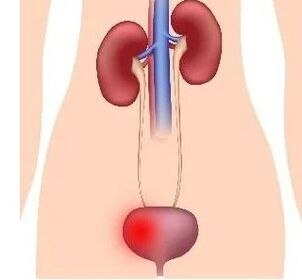
Bacterial agents entering the bladder cavity is possible in three ways:
- The ascending path- through the urethra (urethra). The main role in this version of the penetration of microorganisms belongs to the anatomical and morphological features of the female urinary tract: a short and wide urethra, closely dispensed with the anus and vagina.
- Downward path- From the kidneys. This option develops as the course of renal inflammation, for example, chronic pyelonephritis.
- Hematogenic path- The rarest option is established when cystitis occurs immediately after infectious diseases, or when another source of purulent infection in the female body is detected. There is also a probability of bacterial microflora in the bladder due to the presence of anatomical anastomoses (connections) between the lymphatic vessels of the genital organs and the bladder, subject to inflammatory changes in the above.
The most common causative agent of the inflammatory process of the bladder is the E. coli (in 4 of 5 cases, which is associated with the aforementioned anatomical and morphological characteristics and the presence of this microflora in the intestine).
Less commonly, cystitis is associated with Staphylococcal, streptococcal and Enterococcal microorganisms. Gram -negative sticks cause inflammation of the bladder due to instrumental and surgical interventions.
Recently, the incidence of cystitis associated with fungal microorganisms, the simplest and viruses has increased.
Only the introduction of infectious microorganisms is not enough for the development of a full inflammatory response in the bladder, because the body contains resistance mechanisms to the action of pathogenic flora.
Cystitis development factors
Thus, in addition to the etiological factor, factors such as::
- disorder of hemodynamic function(blood circulation) of the pelvic organs and, in particular, the bladder;
- Disorder of the excretory function of the bladder(stagnation of urine);
- inhibition of various immune links of the body(lack of vitamins, exposure to low temperatures, stress, increased fatigue, etc. );
- Passionate effects of biochemical agentsand exchange products that are released in the urine to the structure of the wall of the bladder;
- exposure to radiological rays;
- non -compliance with hygieneexternal genitalia and random sexual intercourse;
- pathology of the gastrointestinal tract, in the presence of which the microflora accumulates and increases its activity, which subsequently enters the urinary tract;
- Regular shifts of hormonal metabolismwhich leads to the lack of tone of the urethra and creates the best conditions for infection.
The first symptomatic manifestations of cystitis in women
The clinic of acute cystitis in a woman is characterized by a sudden beginning and a pronounced symptom-complexWith:
- The appearance of frequent urination (Pollakiuria)which is characterized by a frequency at least once every 60 minutes and small volumes of the released urine; With the development of frequent imperative urges, patients are not able to control and maintain urine;
- Dysuria (violation of urination)accompanied by pain in the Hypogastric region (in the lower abdomen). With the development of the degree of inflammatory process in the wall of the bladder, these symptoms progress: the more it is developed, the more often the urge to urinate and the more intense pain;
- Itching in the urinary tractarising during the act of urination. Develops due to exposure to the mucous membrane of the urinary tract products of metabolism of microorganisms that caused inflammation of the bladder;
- The appearance of blood dropsat the end of the urination act;
- The appearance of clouding of urine, due to the ingress of a large number of blood cells (leukocytes and red blood cells), bacterial microflora, cells of the surface epithelium of the internal wall of the bladder;
- Such patients are not characterized by a change in the general condition.The temperature indicators of patients are characterized by normal or slightly increased (Low-Gradu) numbers. Scientists associate this with the fact that the mucous membrane of the bladder practically does not suck in the metabolic products of microorganisms, which, having entered the blood, usually lead to intoxication of the body and the development of characteristic symptoms of inflammation.
The connection of the sudden symptoms and preceding hypothermia of the woman’s body that has appeared. Phenomena of acute inflammation can sometimes be observed for 2-3 days and independently disappear without the use of therapy.

Nevertheless, most often this process takes more than 6 days, sometimes up to 15 days. The presence of a disease in a later date, subject to the appointment of therapy, requires the appointment of additional examination methods in order to identify the concomitant pathologies of the body.
Characterization of pain with cystitis in women
In patients with acute cystitis, a different degree of severity of pain syndrome is observed:
- In the light course of the inflammatory process, patients feel insignificant severity or pain in the lower abdomen.Sensitive pains at the end of the urination act accompany the moderate Pollakiuria. With the further development of the inflammatory process, the intensity of pain increases. Subsequently, this syndrome accompanies the beginning or whole act of urination. The pain in becomes unrelated with the act and acquires almost constant in nature, it is accompanied by very painful palpation over the projection of the bladder.
- In a situation where heavy cystitis developed, patients have to urinate at least 2-3 times per hour, which is accompanied by significant pain syndrome and the appearance of blood discharge from the urethra at the end of the act. Pain significantly worsens the quality of the patient’s life, because they do not disappear throughout all days.
The presence of blood cells and blood in the urine with cystitis (hematuria syndrome)
When an inflammatory process develops in the walls of the bladder, it affects the fabric areas near the confluence of the ureters and the urethra exit. The tissue becomes loose and bleeding.
This is manifested by the appearance of micro- and macrohematuria (or blood) in the urine, which is often observed at the end of the urination act (terminal hematuria).
One of the most severe forms of acute cystitis is hemorrhagic. This type of inflammation occurs with a significant penetration of red blood cells (red blood cells) from the bloodstream of the nourishing arteries into the bladder cavity.
This option is possible in case of increased permeability of the walls of blood vessels (condition for anemia, vitamin deficiency, disorders in the operation of the blood system) or damage to the above walls with bacterial cells (usually streptococcal flora). The red blood cells that have fallen into the bubble cavity stain urine in the bloodstone.
When hematuria occurs, the doctor is obliged to carefully conduct differential diagnostics between acute cystitis and complicated acute form - hemorrhagic cystitis. For this, additional examination methods are prescribed, the type of lesion is clarified and the most correct scheme of therapy is selected.
Features of the course of acute and chronic cystitis in women
Sharp cystitis
Summing up the above information, one can distinguish the sharp onset of the disease and the presence of a certain symptom complex for acute cystitis:
- frequent urination in small portions,
- Pain syndrome of various nature,
- itching that is associated with the act of urination,
- the appearance of blood drops at the end of the act,
- The unchanged general condition of the woman.
With a true and timely diagnosis, the pathological condition is cured within 6-10 days. In the absence of improvements after the 15th day of the course of the disease, it is worth thinking about the chronization of inflammatory changes.

In addition to hemorrhagic, there are two more forms of complicated course of acute cystitis:
- Gangrenous.The gangrenous form is rarely found and occurs due to impaired blood supply or innervation of the bladder. Clinically, such a cystitis is manifested by difficulty urination, accompanied by pain, high body temperature, pain in the sacral region. The process is extremely dangerous to the development of formidable complications, such as peritonitis and requires the rapid takeing of measures for treatment.
- Phlegmonous.Phlegmonous form is manifested by significant intoxication of the body, high body temperature and is accompanied by the release of a small amount of urine (oliguria). Urine, with such a complicated current, acquires a putrefactive smell, muddy character, flakes of fibrin formations, blood admixture.
The duration of the course of pathology in the case of the development of complicated forms increases significantly.
There is another form of cystitis - interstitial.It is characterized by inflammation of all urine bubble membranes. The clinic is dominated by sharply rapid urination, reaching up to 180 times a day, active complaints of severe pain in the Hypogastric region when filling the bladder and its regression after the urination act. The capacity of the bubble is significantly reduced, as a result of which the above symptoms occur.
Chronic cystitis
Chronic cystitis, in contrast to acute, rarely occurs as an primary pathology and in most cases is a secondary complication of the course of existing pathologies of the bladder, kidneys, urethra.
Given this fact, it is necessary to carefully examine the body for the presence of the above pathological changes, as well as exclude or confirm the specific origin of microorganisms - tuberculosis stick, invasion of trichomonas.
Clinically, chronic cystitis is manifested either by a continuous course with moderate differences in complaints and clinical analysis of urine, or in the form of a recurrent pathology with periods of exacerbation (similar to the clinic of acute cystitis) and complete regression (with the absence of any manifestations of the pathological process).
Thus, the objective manifestations of chronic cystitis correspond to such in the acute process. They correlate with the common protective properties of the body, the etiology of a bacterial agent that caused an infectious process, and the degree of severity of inflammation. Pain, frequent urination, itching, the presence of blood and clouding of urine are less pronounced with constant course and correspond to the acute process with the recurrent course of chronic cystitis.
Due to the lesion of the inflammatory reaction of the mucosa, the edema of all layers of the urinated wall and the increase in intrapacear pressure created all conditions for the formation of vesicular-memorial reflux, i. e. casting fluid from the bladder back into the ureter (connects the kidneys and bubble).

The doctor-urologist is engaged in the verification of the diagnosis and the purpose of therapy for cystitis.
In order to correctly diagnose inflammatory pathology, it is necessary to clearly fix the patients' complaints and her history (which preceded the development of pathology).
Clinical manifestations are quite specific and can immediately indicate the presence of this disease, however, it is necessary to carefully conduct differential diagnosis between all types of cystitis, as well as from other pathologies of the bladder and diseases of the abdominal organs.
From the anamnesis, data on the stresses and influences of low temperatures, drugs taken, as well as other lesions localized in the pelvic organs and the genitourinary system, will be useful.
After clarifying complaints and an anamnesis, the clinical (general) urine analysis will be able to help in the verification of the diagnosis - increased levels of white and red blood cells will be detected in it (leukocytes and red blood cells, respectively).
To identify the type of bacterial microorganism that caused the inflammatory process, urine is sowing to special nutrient media, which can be used in the future to choose the most effective antibacterial drug.
Before the urine fence for bacteriological examination, it is necessary to qualitatively treat the area of the external genitalia with an antiseptic solution. Conducting cystoscopy in the presence of acute inflammatory reaction is contraindicated.
In order to diagnose chronic cystitis, along with the collection of complaints and data on the anamnesis, cystoscopy helps during remission. This will establish all the necessary characteristics of an inflammatory disease. With this manipulation, it is possible to take biopsy material-the urine-bubble mucous membrane. Also, to identify chronic cystitis, an X -ray study with contrast is recommended.
























